Science & Technology, New Zealand (Commonwealth Union) – Drug resistance to various diseases has been a serious concern for health experts across the world. The over prescription of certain drugs and the evolution of many strains to resist drugs over time have been primarily blamed for drug resistance.
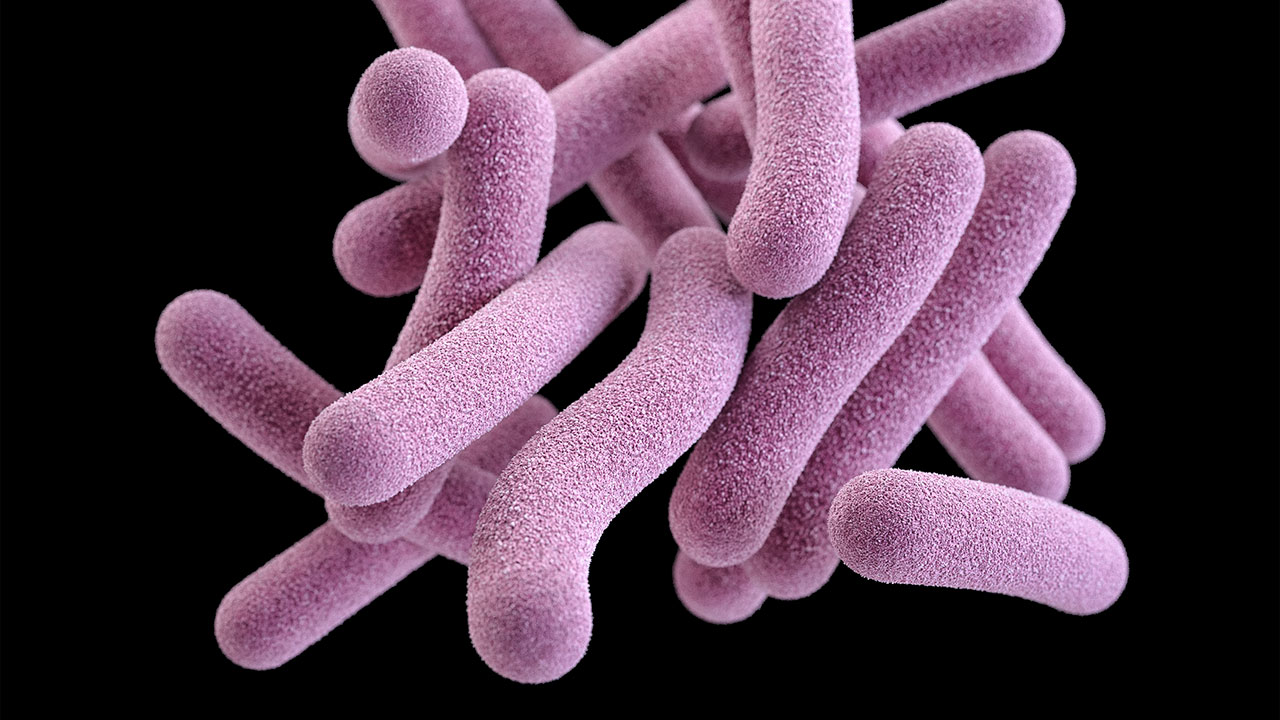
Tuberculosis (TB), is an infectious disease where the bacterium Mycobacterium tuberculosis is responsible. TB primarily affects the lungs, but it can also affect other parts of the body such as the kidneys, spine, and brain. A major challenge in treating TB is drug resistance. Drug resistance can occur when the bacteria that cause TB are able to survive and reproduce despite treatment with one or more antibiotics.
Scientists at the University of Otago have found new ways to treat antibiotic-resistant strains of TB, paving the way for new approaches for tackling the disease that leads to roughly 4,000 fatalities per day.
PhD candidate Natalie Waller as well as Senior Author Dr Matthew McNeil, of the Department of Microbiology and Immunology led the study. The scientists identified antibiotics capable of rapidly destroying drug resistant strains of TB and when combined could halt drug resistance from taking place completely.
TB is a major global health problem, with an estimated 10 million cases each year. Symptoms of the disease can vary depending on the part of the body affected, but common symptoms of pulmonary TB include a persistent cough, fatigue, fever, night sweats, and weight loss. TB can also cause damage to the lungs, leading to complications such as respiratory failure. In New Zealand around 300 cases are diagnosed annually.
TB is diagnosed through a combination of tests, including a chest X-ray, a sputum test to detect the presence of the bacteria, and a skin or blood test to determine if a person has been exposed to the bacteria.
The issue of drug-resistant strains of the disease, which are difficult to treat and with a shortfall of treatment options have increased at an “alarming rate” according to researchers.
Dr McNeil indicated the need not only for new drugs, but improved drug combinations capable of enhancing the treatment success and avoid more spreading of antibiotic resistance.
He further pointed out that, antibiotic resistance leads to lower sensitivity, however in certain cases becoming resistant to one antibiotic may lead to a pathogen with increased sensitivity to other completely unrelated antibiotics. But, the phenomenon of collateral sensitivity was primarily unexplored in TB, until the present.
Dr McNeil also pointed out that its very hardy, resilient and difficult to evaluate in the lab due to its dangerous pathogen that multiples very slowly.
“To overcome this, our study used a weakened non-virulent strain of Mycobacterium tuberculosis that cannot cause disease or survive outside of the lab to generate strains that were resistant to different antibiotics,” explained Dr McNeil.
The scientists then found out if the drug-resistant strains of the bacterium had either been elevated or had lower sensitivity to other antibiotics.
“We wanted the results of our work to have the greatest chance for clinical impact. For this reason, our study placed an emphasis on drugs that are either clinically approved or in pre-clinical development,” added Dr McNeil.
“Excitingly this work identified a number of instances in which a particular drug-resistant strain was more sensitive to antibiotics that targeted a completely unrelated pathway. We then showed we could use these specific drugs to rapidly kill drug resistant strains as well as design unique drug combinations that prevented the emergence of drug resistance.
Dr McNeil also indicated that work will now be required to focus on further implementing these findings into in animal studies.
“There is still work to do, but this is certainly a significant step in the fight again anti-microbial resistance.”