Health & Medical, UK (Commonwealth Union) – Three young patients who had relapsed T-cell leukemia have received treatment with base-edited T-cells, as a component of a ‘bench-to-bedside’ partnership between the University College London (UCL) along with the Great Ormond Street Hospital for Children (GOSH).
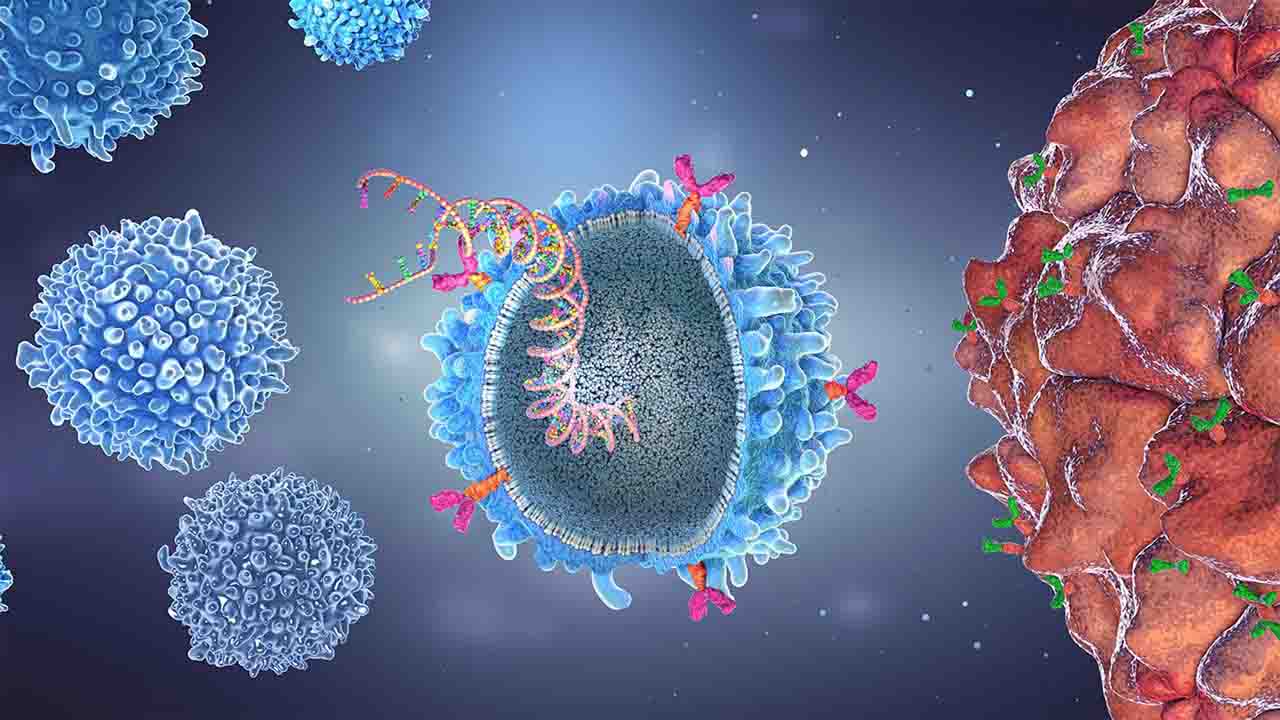
Data obtained from the NHS clinical trial, appeared in The New England Journal of Medicine with funds from the MRC, exhibiting the way donor CAR T-cells were engineered with the application of cutting-edge gene editing technology to alter single letters of their DNA code so they will be capable of tackling leukemia.
The accounts of three patients who underwent cell therapy are shared, including the story of 13-year-old Alyssa from Leicester. She made history last year as the world’s first individual to receive treatment for T-cell acute lymphoblastic leukemia (T-ALL), in a clinical trial. Symptoms for the condition are usually, Fatigue, Easy bruising or bleeding, Pale skin, Frequent infections, fever, enlarged lymph nodes, and spleen among others.
Once, this form of cancer affecting white blood cells is treated with chemotherapy, if it returns, clearing it becomes challenging.
Remarkably, within just four weeks of receiving the specialized cells, Alyssa’s leukemia became undetectable. She subsequently underwent a successful bone marrow transplant and, almost a year later, continues to thrive at home, enjoying good health.
Similarly, another teenager achieved remission from leukemia within a comparable timeframe and is currently recuperating at home following their transplant. Regrettably, the third child experienced complications with serious infections despite responding to CAR T-cell therapy. Consequently, the family, in agreement with the clinical team, decided to transition to palliative care.
The groundbreaking base-editing technology employed in this pioneering human application was conceptualized and developed by a team of researchers at UCL. The project was spearheaded by Professor Waseem Qasim (UCL Great Ormond Street Institute of Child Health and Honorary Consultant at GOSH), in collaboration with Dr. Robert Chiesa and the Bone Marrow Transplant/CART/Haematology teams at GOSH.
The project is backed by Wellcome and the National Institute of Health and Care Research (NIHR).
Professor Waseem Qasim, who is a Professor of Cell and Gene Therapy at UCL, says “It’s nice to be able to see the fruits of a long period of work coming together from multiple teams and being brought into play for new treatments. It’s still early, and we need more follow-up and to treat more patients to know how it might impact treatments long term.”
Dr Robert Chiesa says “It is really crucial that children affected by cancer who failed standard of care have access to innovative strategies in the context of clinical trials such as this. A research hospital such as GOSH offers the ideal setting for developing experimental approaches that might offer hope to children with otherwise very poor prognoses. This is possible due to the dedication of scientists, doctors, nurses, and allied professionals working for these children and their families.”
For the production of banks of ‘universal’ anti-T-cell CAR T-cells for the research, where scientists utilized healthy donor T-cells, put together by the Anthony Nolan registry. This was followed by the cells utilizing ‘base editing’, where the activity includes chemically transforming single nucleotide bases that take instructions for a particular protein, in order to block them being formed.
Some of the steps involved taking away receptors present so that T-cells from a donor are bankable and utilized with no matching making them ‘universal’.
Taking away a ‘flag’ known as CD7 which marks them as T-cells. In the absence of this process, the T-cells may destroy each other.
Removing a second marker called CD52, rendering the edited cells undetectable by certain potent drugs administered to patients during the treatment process.
Incorporating a Chimeric Antigen Receptor (CAR) into the T-cells, which recognizes the CD7 T-cell receptor found on leukemic T-cells. This addition equips the cells to combat T-cell leukemia by targeting CD7.